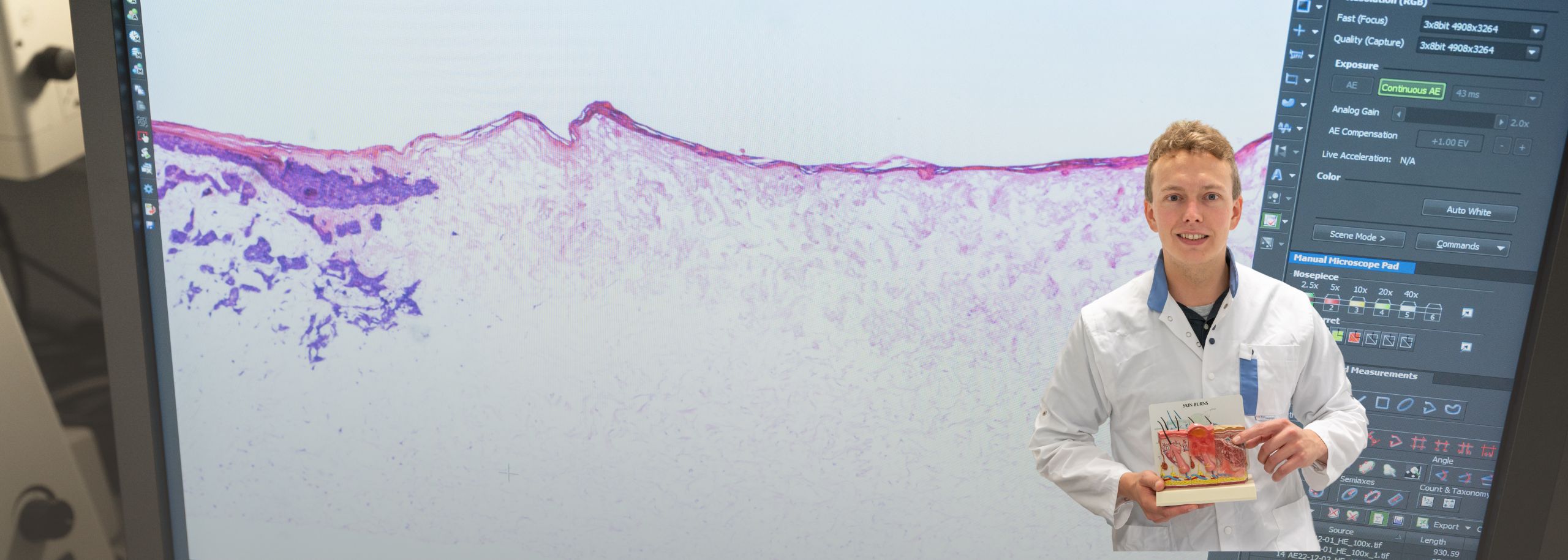
Patrick Mulder is a biomedical researcher. From the Vereniging van Samenwerkende Brandwondencentra Nederland (Association of Collaborating Burn Centers), he works on developing a faster and better way to heal burn wounds. And that is urgently needed because burn wounds cause a lot of damage to the body. They often come with a severe inflammatory reaction that can hinder healing and lead to more scars. Scientists and doctors still don’t have control over this inflammatory reaction – and that’s what Patrick and his fellow researchers are trying to change.
When you have the flu, you get a fever. It makes you feel unwell. Fever is part of your body’s defense against a pathogen. Something similar happens with burns, even without a pathogen. Patrick explains, “If you have a wound, your body responds with inflammation. That’s useful: your body clears dangerous invaders and initiates the healing process. However, the inflammatory reaction in burns is often so intense and prolonged that it hinders the healing process.”
Control over the inflammatory reaction
You can’t completely eliminate the inflammatory reaction because it serves an important function. However, in the case of burn wounds, this intense reaction often lasts much longer than necessary. In his previous research, Patrick and his colleagues mapped out the different inflammatory cells. In this study, they focus on the function of these cells. Patrick says, “We are working to better understand this inflammatory reaction. At the same time, we are optimizing our skin models so that in the final stages of the research, we can test drugs to control the inflammatory reaction.”
Square centimeters of cultivated human skin
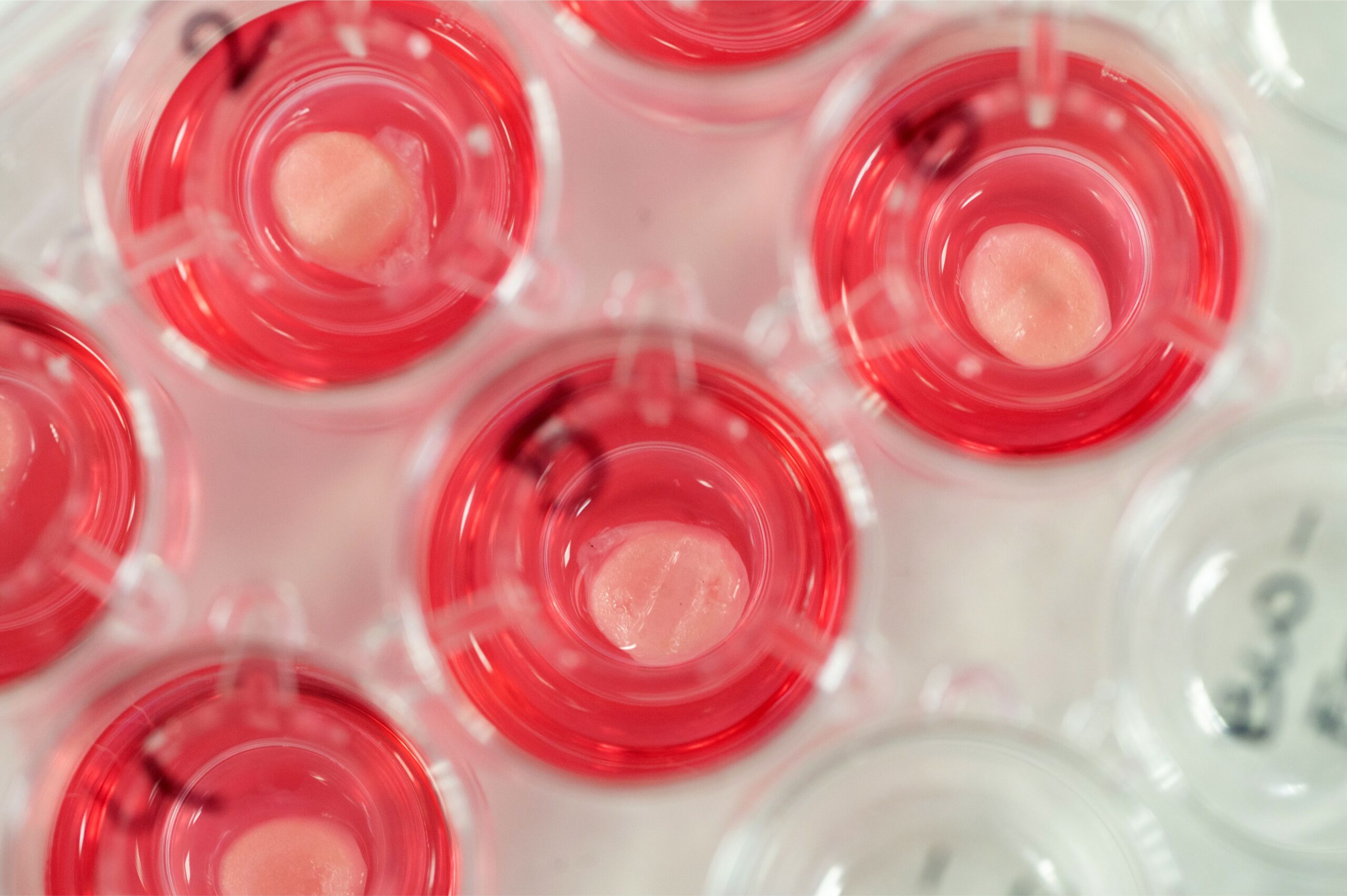
“What is unique about our research is that we have created a human skin model specifically for burn wounds,” says Patrick. “The model consists of pieces of cultivated skin. We create these pieces by letting skin cells grow on a mat made of collagen, a crucial component of our skin. After three weeks, we have small pieces of skin about a square centimeter in size, which look like normal skin under a microscope. This way, we can replace a lot of laboratory animals when we start testing drugs. And here too, we are in uncharted territory: currently, the options to treat inflammation in burn wounds are limited. That’s why we are looking for ways to control inflammation and prevent infections. Ultimately, this will lead to better and faster wound healing.”
The animal-free model of the human skin
No change without alternatives

“If you don’t provide alternatives, nothing will change. Our skin model is not only an alternative to animal testing but also better mimics human skin.” – Patrick Mulder, researcher at Vereniging van Samenwerkende Brandwondencentra Nederland